Over the past week, a few clients have asked the difference between dental decay/holes in the teeth, and gum disease. Are they the same bacteria? Is it because the bacteria are eating the teeth and gums away? Will cleaning the teeth be enough to prevent them from starting or progressing?
Over the past week, a few clients have asked the difference between dental decay/holes in the teeth, and gum disease. Are they the same bacteria? Is it because the bacteria are eating the teeth and gums away? Will cleaning the teeth be enough to prevent them from starting or progressing?
Yes, GUM DISEASE and DENTAL DECAY both are very different in their pathology, presentation and treatment, and dentists have devoted many years studying this stuff. So, below is a quick summary of how they differ from each other.
Interestingly, if left unattended, they both have the same outcomes – loss of the teeth. So take good care of them pearly whites!
About Dental Decay and Gum Disease
Primarily affects the hard structures of the teeth, i.e. the enamel and dentine. When more advanced, it can affect the pulp (nerves and blood supply) within the tooth.
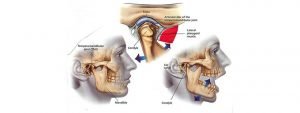
Primarily affects the gums surrounding the teeth. When more advanced, it can affect the ligaments and the bone (alveolar bone) surrounding the teeth.
Enamel: The outer shell of the tooth (very hard) made of hydroxyapatite
Dentine: the bulk of the tooth under the enamel, including the root
Pulp: the nerves and blood supply of the tooth.
Demineralisation: the dissolution of the enamel and dentine.
Dental caries: cavity formation in the enamel and dentine, cause by demineralisation.
Pulpitis: inflammation of the pulp. (Can be reversible, or irreversible - this is when it is serious)
Endodontics: The study of the root canal system
Prosthodontics: The study of restoring the teeth
Periodontium: 4 separate structures described below:
Gingivae - the gums
Alveolar bone, and Cementum - Bone surrounding the roots of the teeth
Periodontal ligament - attachment of the roots of the teeth to the surrounding alveolar bone
Gingivitis: inflammation of the gums
Periodontitis: disease affecting the periodontium (this is when it is serious)
Plaque: layer of bacteria
Calculus/Tartar: Hardened/calcified plaque
Periodontology: The study of the periodontium
Streptococcus mutans, Lactobacillus
Lots of them:
A. actinomycetemcomitans, P. gingivalis, P. intermedia, B. forsythus, C. rectus, E. nodatum, P. micros, S. intermedius and Treponema sp.
The bacteria in the mouth utilizes sugars/carbohydrates from our diet to produce acid. These acids erode/demineralise the enamel and dentine, causing holes in the teeth
The imbalance of bacteria (many theories) in plaque irritates the gums causing inflammation. If left as it is, the inflammation progresses to destroy the periodontal structures.
I am text
In early stages, it starts as a white spot lesion on the enamel.
As it progresses, the white spot lesions start to cavitate and turn into holes.
Sensitivity to hot and cold stimulus
The most common areas affected are the biting (occlusal) surfaces of the teeth and in between the teeth (inter-dental spaces).
In gingivits, the gums will appear red (instead of pink), swollen, and bleeds readily (eg when toothbrushing).
Plaque and calculus present
As it progresses to periodontitis, the attachment of periodontal ligament and alveolar bone is destroyed/lost, resulting in receding gums, pockets, and loosening of the teeth and bad breath.
block. Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Irreversible pulpitis: occurs when the decay reaches the pulp and infects it.
The tooth is broken down.
The pain usually does not settle (for hours) even when the stimulus is removed. Pain can occur spontaneously.
Swelling on the gums next to the tooth due to an abscess (pus)
Poor oral hygiene - lots of plaque and calculus around the gums and teeth
Swollen gums due to abscess (pus)
Periodontal pocketing (loss of the alveolar bone structure - causing the gums to be unattached)
Subginigival calculus: Calculus forming inside the periodontal pocket
Pain and looseness when pressure is applied on the tooth
No white spot lesions or holes.
Gums are stippled, pink, knife edged, and don't bleed.
Teeth are firm.
Early stages:
Fluoride varnishes/gels
Fissure sealants
If the cavity is restorable:
Fill it with a filling
Placed a crown over it
Irreversible pulpitis:
Root canal treatment
Take it out
Gingivitis:
Remove the plaque and calculus with an ultrasonic-scaler
Periodontitis:
All of the above
Periodontal surgery
Take it out
Regular visits to the dentist!
Reduce amount and frequency of sweet and sticky foods
Avoid juices and fizzy drinks. These are both acidic and sweet! Use a straw.
Chew sugar free chewing gum (this stimulates saliva flow and can neutralize the acids)
Use a fluoride toothpaste daily. Fluoride helps strengthen the tooth surface
Regular visits to the dentist!
Remove plaque by using an electric toothbrush, interdental brushes, superfloss, waterpik, etc...
Concentrate on the gum margins (where the gums meet the teeth), not just the tooth itself
Quit smoking!
If you wear dentures, keep them clean and don't wear them at night